Glioblastoma multiforme (GBM) is rare, but also the most malignant type of central nervous system tumor, accounting for more than 50% of all brain tumors in adults
Our lead drug, Berubicin, is an innovative anthracycline that appears to cross the blood brain barrier to kill tumor cells, representing a potential new treatment for patients with glioblastoma multiforme (GBM).
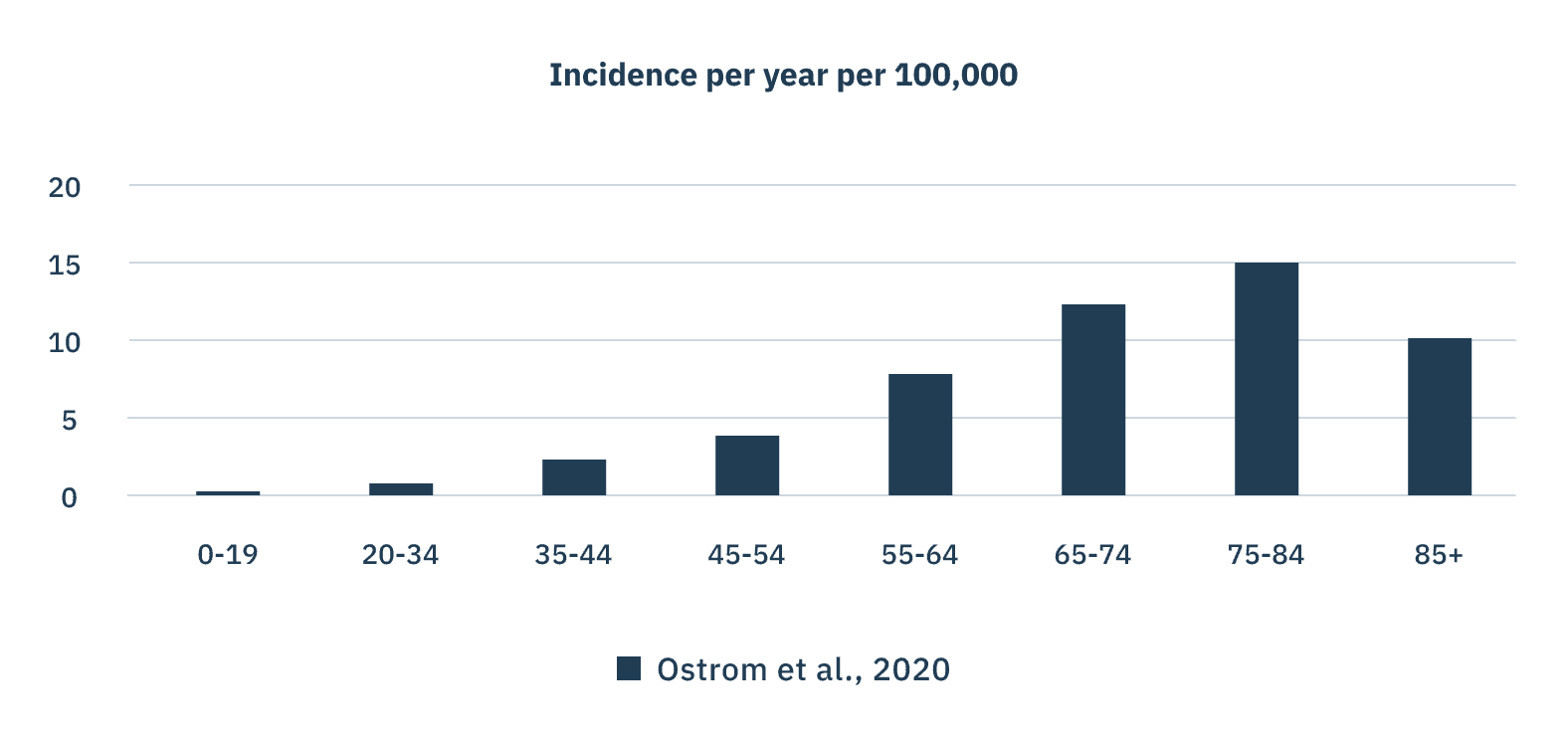
Prevalence of GBM
GBM is a relatively rare disease, affecting approximately 3.2 per 100,000 people. The majority of cases affecting people over the age of 65 years of age, peaking at 84 years. While the incidence of glioblastoma multiforme (GBM) is low compared with other cancers, GBM dwarfs other tumor types in terms of average years of life lost, representing a significant unmet need in oncology.
Treatment options remain limited.
GBM Outcomes
Glioblastoma multiforme (GBM) is rare, but also the most malignant type of central nervous system tumor, accounting for more than 50% of all brain tumors in adults.1
The causes of GBM are largely unknown and the exact origin is rarely identified. Median survival from diagnosis is about 15 to 16 months and only around 25% of patients survive more than 2 years.3
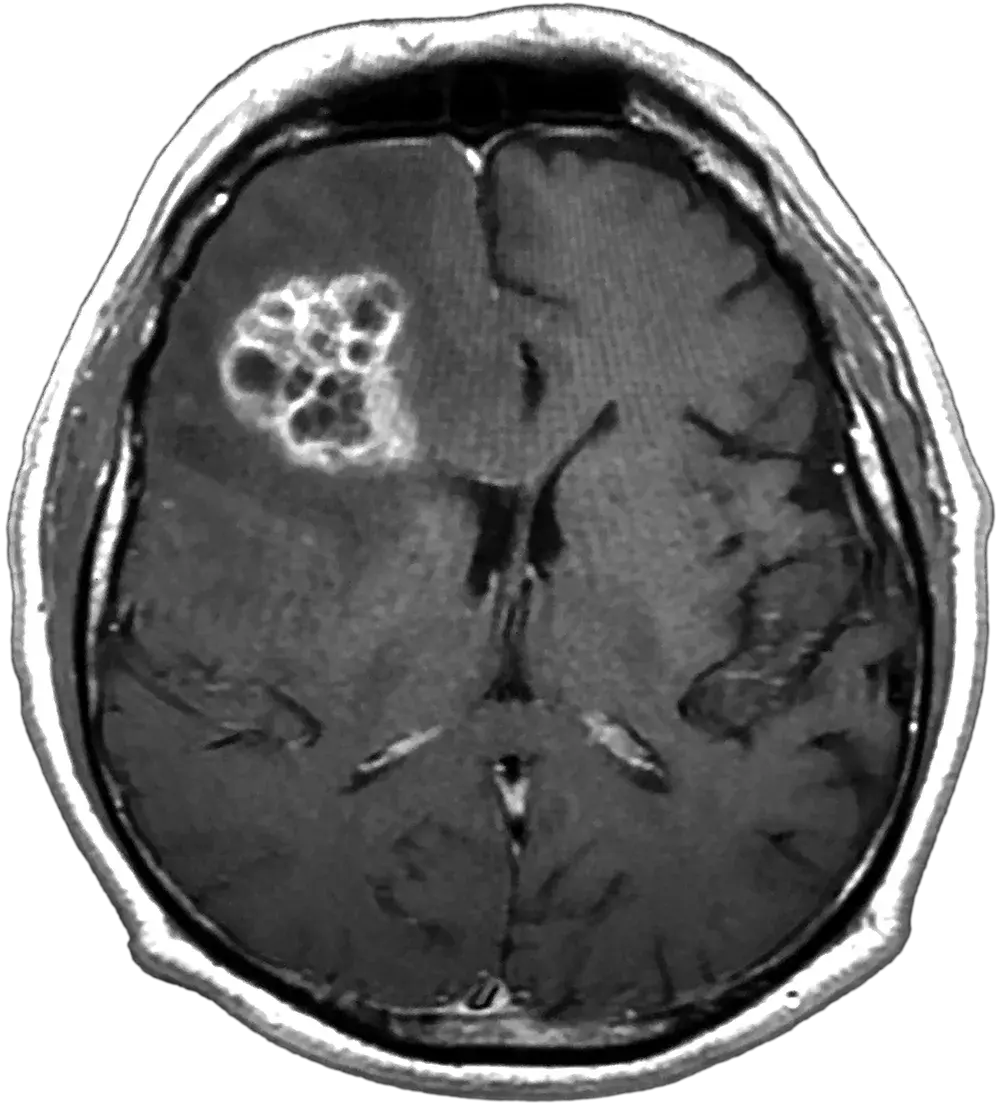
Clinical Presentation of GBM
GBM commonly presents in the cerebral hemispheres with 95% of tumors arising in the supratentorial region (cerebrum). Tumors are usually irregular shaped lesions, creating a typical histopathological pattern on Magnetic Resonance Imaging (MRI) and seen as an enhancing lesion.2,5
The clinical presentation of glioblastoma varies depending on the size and location of the tumor as well as the degree of peritumoral edema, but the most common symptoms are new-onset headache.3 The presence of the tumor within normal brain tissue can cause compression, and infiltration can cause inflammatory changes. These can cause both focal and generalized symptoms such as neurological defects and cognitive and personality changes.
Current Treatment for GBM
The current standard of care for patients with GBM consists of maximal safe surgical resection followed by radiotherapy and chemotherapy with temozolomide.4 Temozolomide is an alkylating agent that works by adding methyl (‘alkyl’) groups to DNA in tumors, causing damage and inhibiting new DNA formation, which prevents further tumor growth. MGMT is an enzyme that antagonizes the effects of temozolomide by repairing the DNA damage. When a gene promoting the transcription of MGMT is methylated, it silences transcription of MGMT, allowing temozolomide to have maximum effect on cell death. If the MGMT promoter is unmethylated, it allows the MGMT enzyme to repair the DNA damage due to alkylating agents such as temozolomide, leading to resistance to its effects and causing an overall poorer survival.
Therefore, although temozolomide is an important drug for the treatment of GBM, there is a critical need for more effective treatment strategies for patients facing the devastating diagnosis of GBM.
Facts About GBM
New cases per year, world wide
Months average survival after diagnosis
Years average age at diagnosis
of patients survive more than 5 years
References
- 1. Rock K, McArdle O, Forde P, et al. Br J Radiol. 2012;85(1017):e729-e733.
- 2. Rodríguez-Camacho A, Flores-Vázquez JG, Moscardini-Martelli J, et al. Int J Mol Sci. 2022;23(13):7207
- 3. Poon MTC, Sudlow CLM, Figueroa JD, Brennan PM. Sci Rep. 2020;10(1):11622.
- 4. Grochans S, Cybulska AM, Simińska D, et al. Cancers (Basel). 2022;14(10):2412.
- 5. Oronsky B, Reid TR, Oronsky A, Sandhu N, Knox SJ. Front Oncol. 2021;10:574012.